Heart disease and the eosinophil
Article Abstract:
Eosinophils (a type of white blood cell) normally constitute from one to three percent of all white blood cells, but the number increases in response to allergic reactions and some infections. The association between a type of heart failure, restrictive cardiomyopathy, and increased levels of eosinophils has been known for over 50 years. Restrictive cardiomyopathy is characterized by rigidity of the ventricular walls, which prevents them from filling properly. Although many organs may be affected, heart dysfunction causes most symptoms and deaths. Differentiation between this form of cardiomyopathy and constrictive pericarditis (gradual scarring of the sac enclosing the heart) is difficult, but magnetic resonance imaging or biopsy may help establish the diagnosis. On rare occasions, it may be necessary to open the chest and observe the pericardium. Acute eosinophilic necrotizing myocarditis, another type of eosinophilic heart disease, is characterized by sudden onset, severe heart failure (of the ventricles), and high mortality. This is different from drug-related hypersensitivity myocarditis, distinguished by a history of sensitivity to drugs, rapid pulse, and sudden and unexpected death from heart failure. The high levels of eosinophils in the blood and tissues of affected patients suggests that these white blood cells lead directly to heart failure. All these disorders are considered to be part of a hypereosinophilic syndrome. Recent research has concentrated on major basic protein, a component of eosinophil granules, which is toxic in high concentrations, and some studies have suggested a relation between eosinophil-granule proteins and myocardial injury. Tissue damage and a high eosinophil count could also be caused by the same virus or allergen. Drug therapy is frequently helpful. Cardiomyopathy with high levels of eosinophils is relatively uncommon, but understanding this syndrome may help researchers to understand a more common disease, idiopathic dilated cardiomyopathy, which may be caused by a viral or toxic response. An antiinflammatory therapy, used for the hypereosinophilic heart disease, may also benefit this condition. (Consumer Summary produced by Reliance Medical Information, Inc.)
Publication Name: The New England Journal of Medicine
Subject: Health
ISSN: 0028-4793
Year: 1990
User Contributions:
Comment about this article or add new information about this topic:
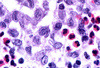
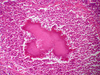
Cardiac localization of eosinophil-granule major basic protein in acute necrotizing myocarditis
Article Abstract:
Eosinophilia describes an increase in eosinophils, a large type of white blood cell, which frequently accompanies inflammatory conditions. It is known to occur with endomyocarditis, an inflammation of the lining of the heart and the heart muscle, and may be caused by a number of conditions, including drug-induced sensitivity, bronchial asthma, and parasitic disease. Drug therapy may be effective in treating endomyocarditis, but sudden acute necrotizing eosinophilic myocarditis is rare, rapid, and fatal. Glucocorticoids, effective in other forms of the disease, are not successful in treating acute necrotizing eosinophilic myocarditis, perhaps because they are usually begun too late in the course of the illness. Two cases describe children, a 14-year-old boy, and a 22-month-old girl, who had virus-like illnesses before developing sudden fatal heart failure. At autopsy, both were found to have acute, extensive necrotizing eosinophilic myocarditis, with no evidence of parasitic infestation. Both patients had received ampicillin (an antibiotic) for the initial infection. The boy received numerous drugs once symptoms of heart failure became apparent. Following the viral infection, the girl was given phenobarbital and phenytoin (Dilantin) for seizures. Although ampicillin and phenytoin have been implicated in hypersensitivity myocarditis, the authors believe the clinical symptoms do not suggest that these drugs played a causative role in the onset of heart failure in these two children. The cause of myocarditis of this type has not been determined. A role for the major basic protein of eosinophil granules has been suggested in Loffler's endomyocarditis, a mild and transient disease. The disease observed in these two patients may be an acute form of Loffler's disease. Because the children died so rapidly, there was no opportunity to try further drug therapies, such as glucocorticoids, which have been effective in the treatment of related disorders. (Consumer Summary produced by Reliance Medical Information, Inc.)
Publication Name: The New England Journal of Medicine
Subject: Health
ISSN: 0028-4793
Year: 1990
User Contributions:
Comment about this article or add new information about this topic:
Pathogenetic mechanisms of septic shock
Article Abstract:
The treatment of patients with septic shock may sometimes be difficult. Septic shock is characterized by hypotension and organ dysfunction. It is caused by the presence of pathogenic microorganisms or their toxins in the blood and other tissues. The development of septic shock starts with the proliferation of pathogenic microorganisms at the origin of infection. These organisms may enter the bloodstream directly, or they may release toxins into the bloodstream. The presence of toxins in the blood can have a serious affect on different organ systems and blood vessels. Death can result from failure of one or more organ system. Very small amounts of endotoxin, a component of the outer membrane of gram-negative bacteria, can cause cardiac dysfunction. Patients with septic shock should be treated with antibiotics. They are frequently admitted to the hospital intensive care unit for treatment.
Publication Name: The New England Journal of Medicine
Subject: Health
ISSN: 0028-4793
Year: 1993
User Contributions:
Comment about this article or add new information about this topic:
- Abstracts: Neonatal infections with coagulase negative staphylococci. Circulatory effects of fast ventilator rates in preterm infants
- Abstracts: L-tryptophan ingestion associated with eosinophilic fasciitis but not progressive systemic sclerosis. Extracorporeal photochemotherapy for drug-resistant pemphigus vulgaris
- Abstracts: Effects of diltiazem or lisinopril on massive proteinuria associated with diabetes mellitus. Improvement of lipid abnormalities associated with proteinuria using fosinopril, an angiotensin-converting enzyme inhibitor
- Abstracts: The epidemiology and natural history of pressure ulcers in elderly nursing home residents. Risk factors for delirium in hospitalized elderly
- Abstracts: Recruitment and retention: successful strategies in critical care. Symposium on successful recruitment and retention strategies in critical care: overview