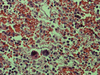
Hypoalbuminemia in patients with multiple myeloma
Article Abstract:
Hypoalbuminemia, or decreased blood levels of the protein albumin, commonly occurs in patients with multiple myeloma, a type of cancer characterized by the invasion of bone and bone marrow by cancer cells that form multiple tumor masses. Multiple myeloma is often associated with anemia or decreased red blood cells, kidney lesions, and high blood levels of the protein globulin. Factors associated with hypoalbuminemia were assessed in 65 patients with myeloma. The blood albumin level was unrelated to patient age or sex, type of myeloma, presence of Bence-Jones protein commonly associated with multiple myeloma, lytic or deteriorating bone lesions, hypercalcemia, increased blood calcium levels, and changes in body weight, and liver and kidney function. Although the blood albumin levels were lower in patients with proteinuria, or the abnormal presence of protein the urine, they were not related to the severity of proteinuria. The albumin level was correlated with the level of monoclonal IgG, which is an antibody or specialized immune protein that normally binds foreign particles; the amount of hemoglobin, the oxygen-carrying pigment of the blood; clinical stage of the disease; and extent of tumor cell growth. The most important factors affecting albumin level were the disease stage and extent of tumor cell growth. Advanced disease was indicated by an albumin level of 29.0 grams per liter or less. The albumin level is mainly related to development of the tumor and is important in the diagnosis and prognosis of multiple myeloma. (Consumer Summary produced by Reliance Medical Information, Inc.)
Publication Name: Archives of Internal Medicine
Subject: Health
ISSN: 0003-9926
Year: 1990
User Contributions:
Comment about this article or add new information about this topic:
Acute toxic effects of sustained-release verapamil in chronic renal failure
Article Abstract:
Verapamil is a drug used to treat high blood pressure, angina, and certain patterns of rapid heartbeat. A new, long-lasting sustained release form of verapamil has recently been marketed for the treatment of high blood pressure. Some of the side effects associated with verapamil include low blood pressure, slow heart rates, confusion, high blood sugars, high blood potassium levels, and high levels of acid in the blood. Four cases of severe toxic reactions to the sustained-release form of verapamil are reported. All four patients had kidney disease, and three required dialysis. The patients were brought to the emergency room and were found to have low blood pressure, dangerously high potassium levels, and evidence of liver damage. Three of the four patients also had excess levels of acid in their blood. All had heart rhythm abnormalities, and one patient sustained a cardiac arrest, from which he was successfully resuscitated. Within hours of supportive therapy, all four patients began to improve and were eventually discharged. Within weeks, their abnormal laboratory values returned to previous levels. These cases suggest that the sustained-release form of verapamil should be prescribed with caution for patients with known kidney disease. (Consumer Summary produced by Reliance Medical Information, Inc.)
Publication Name: Archives of Internal Medicine
Subject: Health
ISSN: 0003-9926
Year: 1991
User Contributions:
Comment about this article or add new information about this topic:
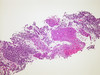
- Abstracts: Pregnancy outcome of patients with uncorrected uterine anomalies managed in a high-risk obstetric setting
- Abstracts: Supplementation of patients with homozygous sickle cell disease with zinc, alpha-tocopherol, vitamin C, soybean oil, and fish oil
- Abstracts: Depression of serum melatonin in patients with primary breast cancer is not due to an increased peripheral metabolism
- Abstracts: Control of immediate postoperative pain with topical bupivacaine hydrochloride for laparoscopic Falope ring tubal ligation
- Abstracts: Multiple myeloma in the geriatric patient. The effect of desmopressin on massive gastrointestinal bleeding in hereditary telangiectasia unresponsive to treatment with cryoprecipitate